Wednesday 14th August 2024
Credits
Report written by Anwen Greenaway
Share the love
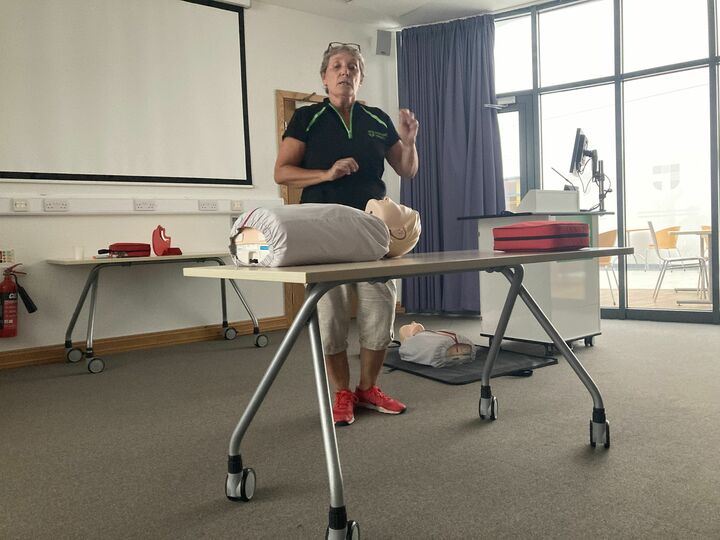
Our Wednesday group session looked a little different last week - We were very fortunate to be offered Basic Life Support training by the lovely Nikki and Elaine at Manor Hospital in Headington. It was a really valuable hour and a half which gave us knowledge and confidence to help in life-or-death situations.
A brief recap of what we covered is below:
The Chain of survival - Early recognition, Early compression, Early defibrillation (ideally in first 5 minutes), early hospitalisation.
Recognising heart attack vs Cardiac arrest.
When someone is having a heart attack they will still be able to talk to you and describe their symptoms. They may complain of pain in their left arm, chest tightness, shortness of breath, and women will often describe a feeling like terrible indigestion.
What to do for a patient with a suspected heart attack:
* Call for help.
* put them into the 'W' sitting position.
* If you know for certain that they are not on any kind of blood thinners give them Asprin 300 mg (crush it if necessary).
* Monitor them closely. If they collapse go to DRS ABC (below).
Someone experiencing a cardiac arrest is effectively dead at that moment. Their heart has stopped. Implement the DRS ABC (detail below). 12% of cardiac arrest patients are saved in the community. It is worth trying CPR and defibrillation - if you do nothing, nothing changes and they definitely die.
DRSABC
D - danger - is it safe?
R - response - do they respond to voice or stimulus?
S - Shout for help - Emphasise the word HELP.
A - Airway - Ensure airway is clear by tilting head back and lifiting the chin.
B - Breathing - assess for breathing for 10 seconds (look, listen, feel), but don't be fooled by 'agonal gasping'. You are looking for regular normal breaths.
C - CPR - start chest compressions.
Top Tips for CPR:
* Get the patient onto a hard surface.
* Aim for compressions in the centre of the chest just below the armpits.
* Aim for compressions about 5cm deep at a rate of about 100-120 per minute. Nellie the Elephant or Stayin' Alive both work well as songs to keep you about the right pace.
* Adults have 3-4 minutes worth of oxygen in the blood, so compressions are the priority. If you aren't happy to give rescue breaths focus on the chest compressions.
* If the patient is in cardiac arrest due to drowning rescue breathes ARE important.
Top Tips for Using a Defibrillator
* One person should continue CPR while the other gets the defibrillator.
* The 999 operator will give you the code to unlock the nearest defibrillator. They will also tell you where your nearest one is. Always go to the one they send you to (they might know your nearest one is out of service, for example).
* Defibrillators on private land should have the code to unlock them on the bottom left.
* SWITCH IT ON! The machine will then tell you exactly what to do step-by-step.
* Continue CPR while the defibrillator is prepared.
* You may need to dry the person off or shave a patch of chest hair to get the pads to stick properly.
* The machine will tell you not to touch the patient (pause CPR too) while it assesses whether the heart is shockable or non-shockable and will advise a shock if appropriate.
* If the heart rhythm is not shockable continue CPR until further help arrives.
* If it is shockable loudly warn everyone around you are about to shock & not to touch patient. “3-2-1 shocking”
What to do if you or someone else is choking
If you are alone and start to choke don't waste time - go and get help from a neighbour or passerby.
Choking protocol:
* 5 effective back slaps
* If that doesn’t work J shape x5
* Then shout for help
* Repeat
* If the patient collapses go to DRS ABC as above
* If they start breathing put in recovery position until help arrives.
Anaphalaxys
In anaphalaxys a massive amount of histamine plummets the blood pressure. Most patients with known allergies will have 2 epi-pens which they should carry at all times.
1. Call for help
2. Get the patient on the floor with their feet up
3. If patient is still responsive get them to administer their own pen
4. If have to administer take off cap push against outer upper thigh. Hold for 10 seconds.
5. Monitor for 5 minutes
6. If there's no improvement after 5 minutes give the 2nd pen in their other leg
7. If the patient doesn't have a pen you should do steps 1 and 2 and closely monitor them until help arrives.
MANY thanks to Elaine and Nikki for giving us this valuable training.
Find your nearest defibrillator here.
DRSABC here.
Discuss this report
Join us on our next session